Table of Contents
- Prolonged Preoperative INR is an Independent Risk Factor for Postoperative Venous Thromboembolism after Neurosurgery
- Risk Assessment of Acute Stroke Patients Developing Symptoms or Testing Positive for SARS-CoV-2 From Admission up to 2 Weeks FOL
- Critical Care Needs Among Acute Ischemic Stroke Patients Who Received Thrombolytic Therapies and/or Mechanical Reperfusion
- Creutzfeldt-Jakob Disease: A Geographic Case Series in the Northeastern United States
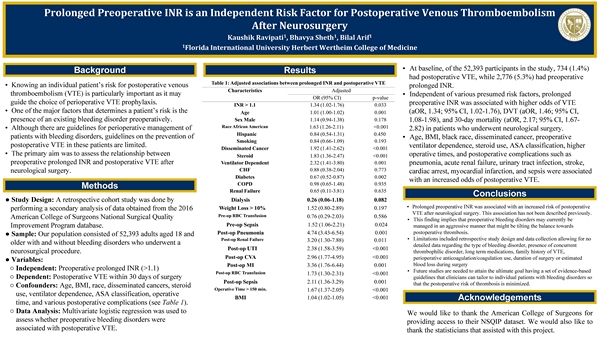
Prolonged Preoperative INR is an Independent Risk Factor for Postoperative Venous Thromboembolism after Neurosurgery
Kaushik Ravipati, Bhavya Sheth, B.S., Bilal Arif, B.S.
Background/Significance
Postoperative venous thromboembolism (VTE) is a risk of all surgical procedures, particularly neurological surgery, and is associated with significant morbidity and mortality. One of the major factors that determines a patient’s risk is the presence of an existing bleeding disorder preoperatively. Therefore, our primary aim was to examine the association between prolonged preoperative INR and postoperative VTE after neurological surgery.
Methodology/Data Analysis
A retrospective cohort study was done by performing a secondary analysis of data obtained from the 2016 American College of Surgeons (ACS) National Surgical Quality Improvement Program database. Our population consisted of 52,393 adults age 18 and older who underwent neurosurgery. The exposure was whether or not patients had a prolonged INR (> 1.1) preoperatively. The primary outcome was postoperative VTE within 30 days of surgery that warranted therapeutic intervention. Odds ratios were estimated using a multivariate logistic regression model.
Findings/Implications
At baseline, 734 (1.40%) had postoperative VTE while 2,776 (5.3%) had a prolonged preoperative INR. Independent of various presumed risk factors, prolonged preoperative INR was associated with higher odds of VTE (aOR, 1.34; 95% CI, 1.02-1.76), DVT (aOR, 1.46; 95% CI, 1.08-1.98), and 30-day mortality (aOR, 2.17; 95% CI, 1.67-2.82), but not PE (aOR, 1.10; 95% CI, 0.70-1.73). Age, BMI, black race, disseminated cancer, preoperative ventilator dependence, steroid use, ASA classification, higher operative times, and postoperative complications such as pneumonia, acute renal failure, urinary tract infection, stroke, cardiac arrest, myocardial infarction, and sepsis were associated with increased odds of postoperative VTE.
Conclusions
Our results suggest that prolonged preoperative INR may be associated with an increased risk of postoperative VTE following neurosurgery. Therefore, these data imply that bleeding disorders may be being managed too aggressively preoperatively, leading to a shift in balance to postoperative thrombosis. If validated by future studies, careful pre- and postoperative planning for patients deemed to be at high risk may reduce postoperative complications.
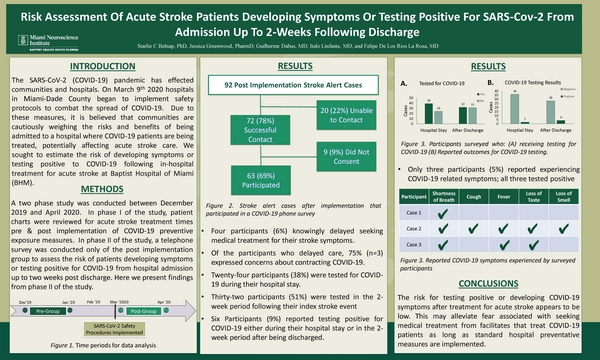
Risk Assessment of Acute Stroke Patients Developing Symptoms or Testing Positive for SARS-CoV-2 From Admission up to 2 Weeks FOL
Starlie Belnap, Ph.D., Jessica Greenwood, PharmD, Guilherme Dabus, M.D., Italo Linfante, M.D., Felipe De Los Rios, M.D.
Background/Significance
The SARS-CoV-2 pandemic has affects communities and hospitals. It is believed that communities are cautiously weighing the risks and benefits of being admitted to a hospital where COVID-19 patients are being treated, potentially affecting acute stroke care. We sought to estimate the risk of developing symptoms or testing positive to SARS-CoV-2 following in-hospital treatment for acute stroke at Baptist Hospital of Miami (BHM).
Methodology/Data Analysis
A two phase study was conducted between December 2019 and April 2020. In phase I of the study, patient charts were reviewed for acute stroke treatment times pre & post implementation of COVID-19 preventive exposure measures. In phase II of the study, a telephone survey was conducted only of the post implementation group to assess the risk of patients developing symptoms or testing positive for SARS-CoV-2 from hospital admission up to two weeks post discharge. Here we present findings of study phase II.
Findings/Implications
We were able to contact 78% (N=72) of acute stroke patients with 87.5% (N=63) of those patients agreeing to participate in the study. Of these, 6% (N=4) reported knowingly delaying to seek medical treatment for stroke symptoms from which 75% (N=3) expressed concerns about contracting COVID-19. Within 2 weeks of discharge, 51% of patients surveyed were tested for COVID-19. Of these, 12.5% (N=3) had a confirmed positive result. One patient was asymptomatic and three patients experienced symptoms. Two patients reported the symptoms began during stroke hospitalization and one stated symptoms developed after discharge. Risk of positive COVID-19 result for the 2-week period following discharge was 6%.
Conclusions
The risk for testing positive or developing COVID-19 symptoms after treatment for acute stroke appears to be low. This may alleviate fear associated with seeking medical treatment from facilitates that treat COVID-19 patients as long as standard hospital preventative measures are implemented.
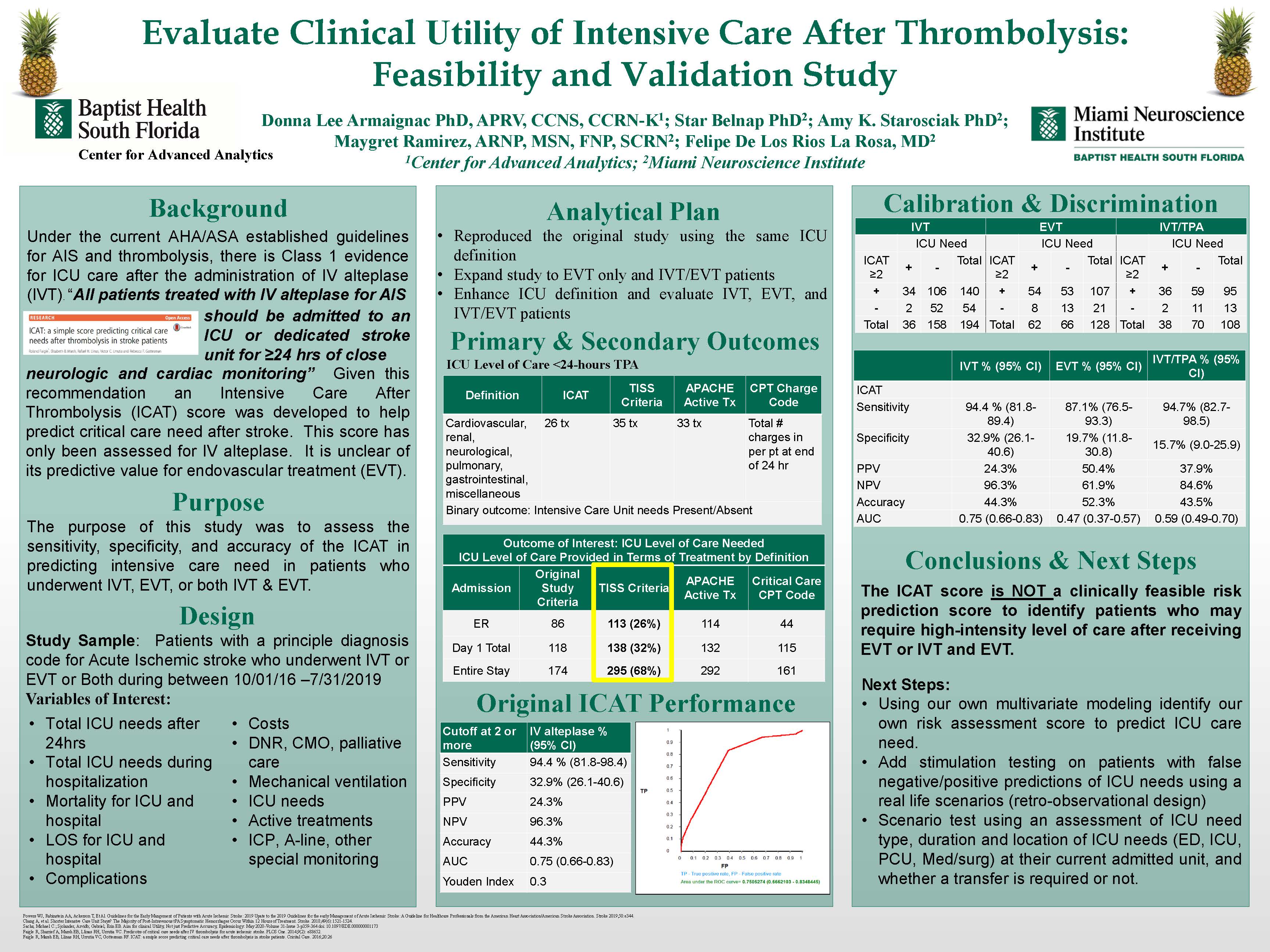
Critical Care Needs Among Acute Ischemic Stroke Patients Who Received Thrombolytic Therapies and/or Mechanical Reperfusion
Donna Lee Armaignac, Ph.D., ARNP, Starlie Belnap, Ph.D., Maygret Ramirez, ARNP, Amy Starosciak, Ph.D., Felipe De Los Rios, M.D.
Background/Significance
Not all patients undergoing tPA or endovascular treatment (EVT) for acute ischemic stroke may require ICU level of care. Intensive Care after Thrombolysis (ICAT) Score developed to predict ICU needs in anterior circulation post tPA patients > 2 predicts critical care needs with 97.2% sensitivity and 28% specificity. The score has not been studied for EVT.
Methodology/Data Analysis
Patients: Adult acute ischemic stroke patients who received thrombolytic therapies and/or mechanical reperfusion at comprehensive stroke center admitted Oct 1 2016- July 31 2019
Design: observational cohort retrospectively calculated ICAT score and examined ICU needs per defined criteria. We calculated the sensitivity and specificity per tPA, EVT or combination treatment groups
Data Source: EHR records, administrative data, benchmarking data files, hospital submitted patient records to registry, critical care database.
Measurements: Sociodemographics, Stroke risk factors, NIHSS parameters at presentation, CT or MRI and pre-defined ICU specific care requirements.
Predicator Variable ICAT Score
Primary Outcomes: ICU level of care required in first 24 hours including: comfort measures only (CMO), DNR, mechanical ventilation, active ICU treatments, number of cases that require active treatment and number of cases that require invasive monitoring of intracranial pressure, blood pressure and require special devices.
Secondary Outcomes: Total intensive care needs of entire stay, ICU and hospital mortality, ICU and hospital LOS, and total complications.
Findings/Implications
433 patients met inclusion criteria. Of these, 198(45.6%) received IV tPA, 128(29.4%) EVT, 104(23.9%) combination treatment. The sensitivity and specificity of ICAT to predict ICU needs were (94.4%, 32.9%), (87.1%, 19.7%), and (94.7%, 15.7%) respectively. The calculated AUC was 0.751, 0.472, and 0.598 respectively.
Conclusions
The ICAT score performs best for those receiving IV tPA with high sensitivity but poor specificity. Many patients undergo unnecessary costly ICU stays. Improved screening tools are required.
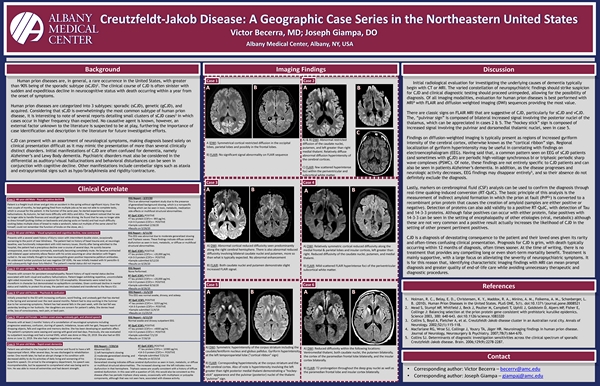
Creutzfeldt-Jakob Disease: A Geographic Case Series in the Northeastern United States
Victor Nicholas Becerra, M.D., Joseph Giampa, D.O.
Background/Significance
Human prion diseases are, in general, a rare occurrence in the United States. CJD has an average age-adjusted incidence of 0.97 per 1,000,000 persons, with greater than 90% being of the sporadic subtype (sCJD). The clinical course of CJD is often sinister with sudden onset of expeditious decline in neurocognitive status and death occurring within a year from the onset of symptoms which include behavior abnormalities, myoclonus, ataxia, or even psychosis.
Methodology/Data Analysis
A total of six patients with CJD (two female and four male) were included between August 2020 and January 2018. Ages ranged from the fifth to seventh decades of life. Key MRI images were of each patient were obtained for comparison and correlation with presentation and serological/clinical testing.
Findings/Implications
The current gold standard for suggesting the diagnosis of CJD is MRI. Characteristic imaging findings are notably seen on diffusion-weighted imaging (DWI) which show progressive signal intensity in the cerebral cortex/striatum (gyral enhancement “cortical ribbon sign”). T2 weighted imaging (T2WI), shows increased signal intensity in the basal ganglia, thalami, and throughout the cerebral cortex. FLAIR sequence can demonstrate a characteristic “pulvinar sign” which involve symmetric increased signal within the thalamic posterior nuclei as well as the “hockey stick sign” where the dorsomedial thalamic nuclei also increase in signal.
Conclusions
CJD is a diagnosis of devastating consequence to the patient and their loved ones given its rarity and often-times confusing clinical presentation. Identifying characteristic imaging findings with MRI can mean prompt diagnosis and greater quality of end-of-life care for the patient while avoiding unnecessary therapeutic and diagnostic procedures.

 Facebook
Facebook X
X LinkedIn
LinkedIn Forward
Forward